Blood Sugar 101

Everything You Need to Know About the Sneaky Culprit Behind Your Mystery Symptoms
Have you ever felt gaslit by your own body?
We’re talking about those afternoon dips in energy that makes you question if you ate lunch at all.
The extra weight you can’t shed no matter how hard you try.
The stifling, sweaty hot flashes that firebomb you in the middle of an important meeting.
Can they tell I’m on fire inside?
The debilitating cramps that leave you hunched over in pain.
And those god-awful bright red, swollen pimples that make you feel like you’ve been plopped right back into puberty.
It’s awful. All of it.
So, we grab our 3PM coffee, pop a Midol, drag ourselves to more circuit training classes, and go on Accutane to blast out our acne. Because we needed relief yesterday.
But what we’re really doing is playing whack-a-mole with our symptoms. Because none of this gets to the root of what-in-the-heck is going on inside our bodies.
What if we told you there’s likely one single culprit wreaking all this havoc across every single part of your body, from your brain to your belly. And that culprit is…blood sugar.
Wait. What’s Blood Sugar?
Blood sugar is exactly what it sounds like - it’s the sugar in your blood, and it’s your body’s main energy source. It also goes by the name “glucose”.
Here’s how it works: the food you eat is broken down mostly into sugar, and it’s this sugar that keeps the lights on and the engine running in your body. Even now, you’re using energy from sugar to read this article.
That’s right… you need blood sugar to learn about blood sugar!
🤯
Now, the reason it’s called “blood” sugar is because the broken-down sugar from your food doesn’t just magically teleport to every part of your body. Your blood is the
highway that transports it to your cells, where it gets burned to create the energy you need to function.
So, to recap, when that sugar’s getting carpooled through your blood to your cells, that’s when it’s called
blood sugar.
Highs and Lows are NORMAL
To be clear, rises and falls in blood sugar are exactly what should be happening in your body. It’s how we digest food, convert it into energy, and burn that energy. Naturally, our blood sugar will fluctuate within a healthy range during that process.
What we’re trying to say is this: Don’t let people scare you into thinking your curve needs to be a flatline! We all know what a flatline means 😵
Here’s what you should be aware of: big peaks and valleys in your blood sugar levels. Especially if they’re persistent. Your body will let you know this is happening through symptoms like fatigue, irritability, nausea, irregular or fast heartbeat, difficulty concentrating, confusion, even nightmares.
The bottom line: when we feel off, it’s because there
is something off. Your body ain’t lying. And it’s probably your blood sugar that’s the culprit.

Hold the phone. I thought only people with diabetes have to worry about blood sugar?
Well, you’re right. They do have to worry about it.
In the United States, about 12% of the adult population is estimated to have diabetes. Think of it this way: if you’re in a room with 10 people, one person will have Type 2 diabetes. (1)
So, what is it exactly?
It’s when your blood sugar is higher than it should be for a long, long time, and the fuel from the food you’re eating may not be getting into your cells, where it can be burned for energy. This leaves your cells feeling starved and unable to function properly.
But diabetes doesn’t just magically happen overnight.
According to the Centers for Disease Control (CDC), more than one-third of American adults - 98 million - are estimated to have prediabetes, with more than 80% of those people having no idea they have it. (2) Prediabetes is when your blood sugar is consistently higher than it should be, but not quite high enough to be considered Type 2 diabetes.
So take a look at the person to your left and your right. Chances are one of you has prediabetes.
😳
We need a new way to monitor blood sugar, here’s why…
Like we just mentioned, most people don’t know they have prediabetes, and oftentimes that’s because it’s downplayed by their doctor.
This is usually how it goes down.
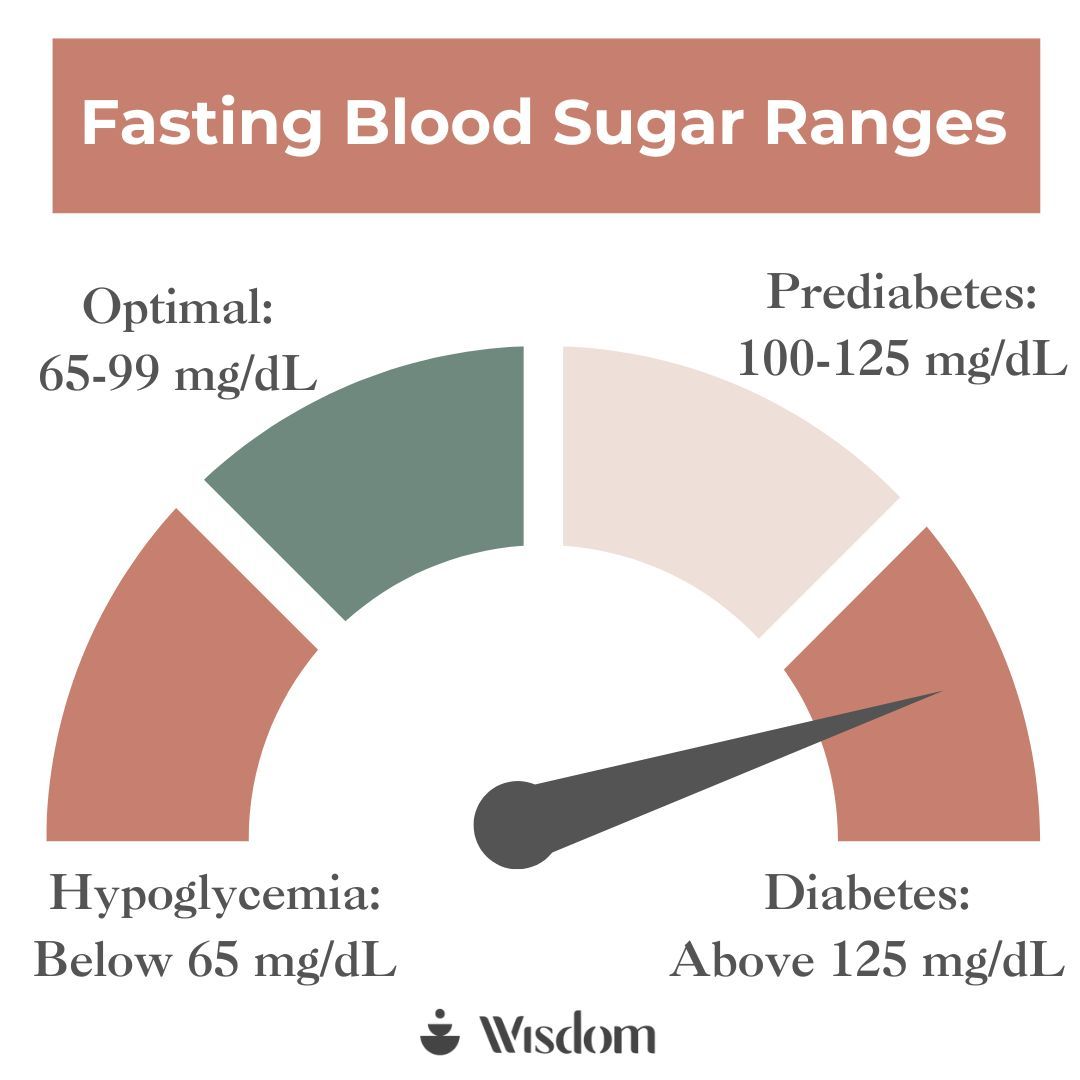
You do your annual exam and they test your fasting blood sugar (the only test doctors use to test your blood sugar levels). It comes back high…and your doctor tells you not to worry, because you aren’t diabetic.
They might add a note to your visit summary saying to “eat healthy, exercise, and manage your weight”, but in the frame of conventional medicine, there’s nothing else they can do until you reach full-blown diabetes. And once that happens, there’s no going back, because there’s no cure for diabetes. Just treatment.
Not only that, but one of the limitations is the
fasting glucose test
itself.
That’s because it only shows us the teeniest, tiniest one-moment-in-time snapshot of what your blood sugar is in the morning on that one specific day.
It doesn’t tell us
anything about what is happening for the rest of the day, week, month, or year.
While you might wake up and have blood sugar levels within the optimal range in that one moment in time, it doesn’t tell us how your body responds to what you are eating later in the day, how you’re sleeping that night, and the stress you’re under the next day trying to meet that work deadline before school pickup. All of those things have a huge impact on your blood sugar.
So even though you came to the doctor saying you haven’t felt great in a while - with chronic things like fatigue, energy surges and dips throughout the day, maybe even hormonal symptoms like acne, or painful and heavy periods - you are told that everything is normal. Because that one moment-in-time snapshot of your blood sugar was normal from your fasting glucose test.
See how it doesn’t add up? Because in reality, your real-time blood sugar is out of whack, causing your entire body to be out of whack. We need real-time blood sugar monitoring to capture the truth of what’s going on (more on that later, so stay with us!).
Let’s take a deeper dive into some of those symptoms and how blood sugar could be the sneaky culprit behind them.
Fatigue
This is what the vast majority of our members come to us to solve: bone-tired fatigue that makes them feel like they’re walking through sand all day.
Sure, it’s not
always related to blood sugar (but, odds are, it is). Other factors include things like iron levels, stress, and quality of sleep. How we eat can also be a big player in fatigue, because… you guessed it… it affects our blood sugar.
Here’s why: when food hits your stomach, your pancreas kicks into gear. The pancreas is responsible for releasing digestive enzymes to help break down your food, but it’s best known for its role in producing (drumroll, please!) 🥁🥁🥁 insulin.
Insulin is a hormone that helps “unlock” the doors to your cells, so the broken-down sugar from the food you just ate can get in.
But what if your fuel can’t get into your cells?
In some cases, your pancreas might not be releasing enough insulin to unlock the doors to your cells OR your insulin might have trouble unlocking these doors altogether. Either way, it causes a jammed door. This leads to broken-down sugar in your blood also getting backed up, causing your blood sugar levels to rise. Meanwhile, the power plant in your cells is left with no fuel to burn.
And when your cells don’t have energy, neither do you.
Weight Management
Let’s be clear about one thing first. Maintaining a relatively stable weight is the most important thing when it comes to weight management and your health. Notice how we didn’t say a specific BMI or body size. Nope. That’s because your body–all of our bodies–change over the course of our lives.
But there may be times you mysteriously get blindsided by 10, 20, 30+ pounds that came out of nowhere, and there’s no amount of weight loss gimmicks or hours spent at the gym that can get them to go away. Meanwhile you may be depriving yourself of important nutrients or rest your body needs to heal and recover.
So, what does that have to do with blood sugar?
Let’s revisit our good friend, insulin. In addition to helping sugar get out of your blood and into your cells, it also signals your body to store fat.
What that means is if you have more insulin running around your body, shouting to cells to store more fat, then that’s exactly what they’ll do. They’re very obedient.
This is why one of the most common (and most overlooked) reasons for our frustration with healthy weight management stems back to our blood sugar. Because when our blood sugar is mismanaged or chronically high, we have higher levels of insulin, which means more fat storage.
Hot flashes
Little fun fact: hormonal imbalances during perimenopause and menopause can impact blood sugar levels.
And, if you’re starting to catch our gist, imbalanced blood sugar can cause your body to start gaslighting you in a number of delightful ways during this already turbulent time of transition in our lives. Sporadic blood sugar is the icing on the cake, causing all of the hallmark symptoms of peri/menopause to be that. much. worse.
For example, hot flashes.
That’s because when you have less estrogen and less progesterone in your body (aka when you’re in peri/menopause), this can lead to worse blood sugar regulation.
And while many issues with blood sugar are related to when it’s too high, it’s actually
low blood sugar that can trigger hot flashes. They are more likely to occur when blood sugar falls between meals, and the frequency of hot flashes are more likely to increase as the time between meals increases. This is why women often experience hot flashes alongside night sweats, further disrupting your sleep.
And if a perimenopausal or menopausal woman experiences blood sugar-related symptoms like hot flashes, it increases her risk for developing diabetes in the future.
The good news is, when women in peri/menopause monitor their blood sugar and work from a personalized care plan (like
the bundle we offer) to keep their blood sugar levels within a healthy range, their hot flashes finally start to sizzle down and cool off. Don’t believe us? Try it yourself!
PCOS
Did you know that Polycystic Ovary Syndrome (PCOS) is a hormonal disease?
It’s caused by an excess of androgen hormones, which can then lead to missed periods and missed ovulation. When ovulation gets skipped, the ovaries can develop many small, fluid-filled sacs called cysts.
If you think that sounds awful, you’re right. It is.
It usually looks like irregular or missed periods, more hair than you might like on the face or body, skin conditions such as acne and skin tags, hair loss (alopecia), weight gain (especially around the belly), and reduced fertility and no ovulation.
What is less well known about PCOS is that it’s also called “diabetes of the ovaries”.
It earned this nickname because the hormonal imbalances that happen with PCOS often lead to insulin resistance. This means that women with PCOS usually make more insulin, but their bodies don’t know what to do with it… which leads to high blood sugar levels… which leads to etc. etc. etc.
This is why personalized blood sugar management can be
such a game changer for women with PCOS. More on that to come later!
Cravings
Back to the pancreas. A little refresher. It makes insulin and glucagon, which are hormones that regulate our bestie, blood sugar.
Insulin lowers blood sugar levels, while glucagon raises them.
When these hormones are unbalanced (which can be caused by a variety of environmental and lifestyle factors), it can lead to high or low blood sugar levels. And we all know what that means: fatigue, weight gain, irregular periods, and (wait for it, there’s another one..) cravings.
Imagine: it’s almost noon, you’re at your wit’s end, and you can hear your stomach announcing its discontent, growling for the whole world to hear.
You
know
you need more than coffee to perk you up before you accidentally tell your boss to jump into the Grand Canyon. But, crap, you have
another video meeting in 5 minutes. You know you need energy, fast. Which the cells in your body shout back to you: sugar! Eat sugar ASAP!
So you (gleefully) grab a chocolate chip cookie that’s been staring at you on your desk for a full hour, calling your name.
You eat the cookie, and it’s amazing. Your energy and attention perk up, and you start to feel like a fully functioning human again. You’re feeling
good. This means the energy (read: sugar) in the cookie is making its way into your bloodstream and is providing your cells the fuel they were clamoring for.
But then 30 minutes later…you crash. You’re right back to square one but this time feeling
more irritable and
more tired. You can’t seem to focus on your boss on the other side of your screen. Is this what they call brain fog? And, here we go again,with your stomach back to rumbling.
So
what happened?
Remember our friend, insulin, and how it helps unlock your cells to let fuel in? Well, it’s also a part of your “fullness” mechanism that lets your brain know you’ve had enough food (aka energy). All that food chatter starts to pipe down.
In the case of the cookie and other “naked carbs”, it gets digested very quickly, causing our blood sugar to rise fast. In fact, it rises so fast, our insulin can’t keep up. It gets backlogged and can’t tell all the cells to open the doors and let all that energy in!
Because of this, we end up with a surge in blood sugar, followed by an even steeper drop. You know…that bottomed out, low energy feeling like you’ve suddenly been hit by a tranquilizer dart.
And if you find yourself feeling hungry again, it’s likely because of ghrelin, one of insulin’s opposing hormones that causes hunger. We like to think of ghrelin as a microscopic, hungry
gremlin…which is coincidentally exactly how you end up feeling when you crash.
Bottom line, if your blood sugar drops too low, those cravings start to ramp up. You know an effective way to avoid that? You guessed it. Keeping your blood sugar in a healthy range, away from those peaks and valleys.
Alas! Meet the Continuous Glucose Monitor 🦸🏽♀️🎉
As we mentioned, the once-a-year fasting glucose test is not the greatest.
And while it’s a good piece of your health puzzle–we shouldn’t throw the baby out with the bathwater–we do need more info to put together the full picture.
Because your blood sugar is a living, breathing thing. It changes in response to
everything from food to sleep to stress. We need to collect that data in real-time to be able to connect the dots and see what keeps your blood sugar levels in a happy, balanced place.
A Continuous Glucose Monitor, or CGM, is a nifty little wearable device our providers use to get to the bottom of
your biology and
your symptoms.
It measures your blood glucose over a period of 14 days, giving us an inside peek into your higher- or lower-than-normal blood sugar fluctuations and what triggers them.
With that data, we can give you a personalized plan to keep your blood sugar in a healthy range–all based on your one-of-a-kind body and your one-of-a-kind blood sugar data.
Future You Will Thank You
Not only is managing blood sugar important for the here-and-now symptoms, it’s also a critical factor to keeping up your long-term quality of life and longevity.
For example, dysregulated blood sugar and particularly high blood sugar over time increase your risk for (3):
- Type 2 Diabetes and Gestational Diabetes
- Heart Disease
- Kidney Disease
- Dementia
In the traditional medical system, it’s difficult to get care
before you receive an official diagnosis, which causes so much frustration and a feeling that you don’t have control over your health. It doesn’t have to be that way.
Get faster answers about
your biology with a one-size-fits you care plan with our brand new
Blood Sugar Bundle. It comes with a CGM + doctor’s review + personalized care plan to flatten your blood sugar curve based on your body and your data. It’s our best price yet at $299, and it’s FSA/HSA eligible. Get started today and future you will thank you.
References
- American Diabetes Association. Statistics About Diabetes.
- Centers for Disease Control. Prediabetes: Could It Be You?
- Cleveland Clinic. Diabetes.