Hormones,
Your Body’s
Communication Pathway
Your body uses hormones for nearly everything. Hormones fluctuate naturally throughout the month, and also as we age. Nearly half of women experience some form of hormone issue throughout their life, which can cause a variety of confusing, and seemingly disconnected symptoms. Conventional medicine considers hormone issues “incurable.” However, that’s misleading. Lifestyle changes can have dramatic effects on our hormones, and it’s more accurate to say hormone issues are not reversible through medication.
Hormone Levels Throughout The Month
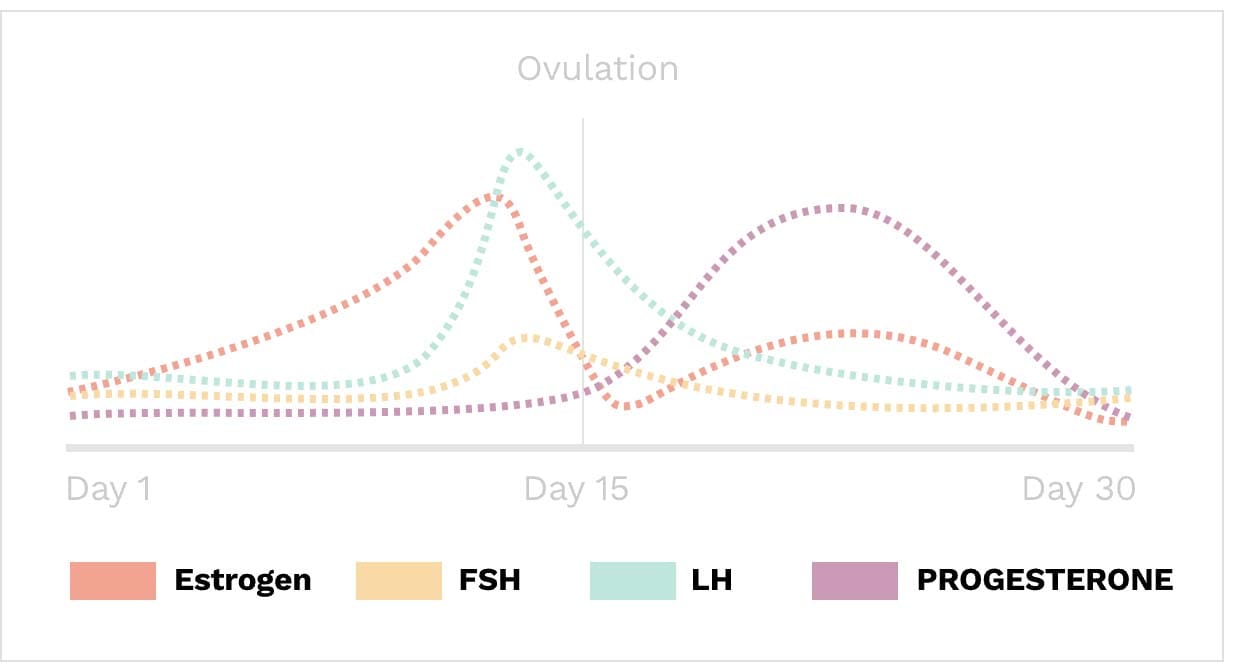
Healthy menstrual cycles have natural hormone fluctuations throughout an individual cycle, with natural peaks. Many women with imbalanced hormones do not have the correct proportion of hormones at a given cycle time, causing a variety of confusing symptoms.
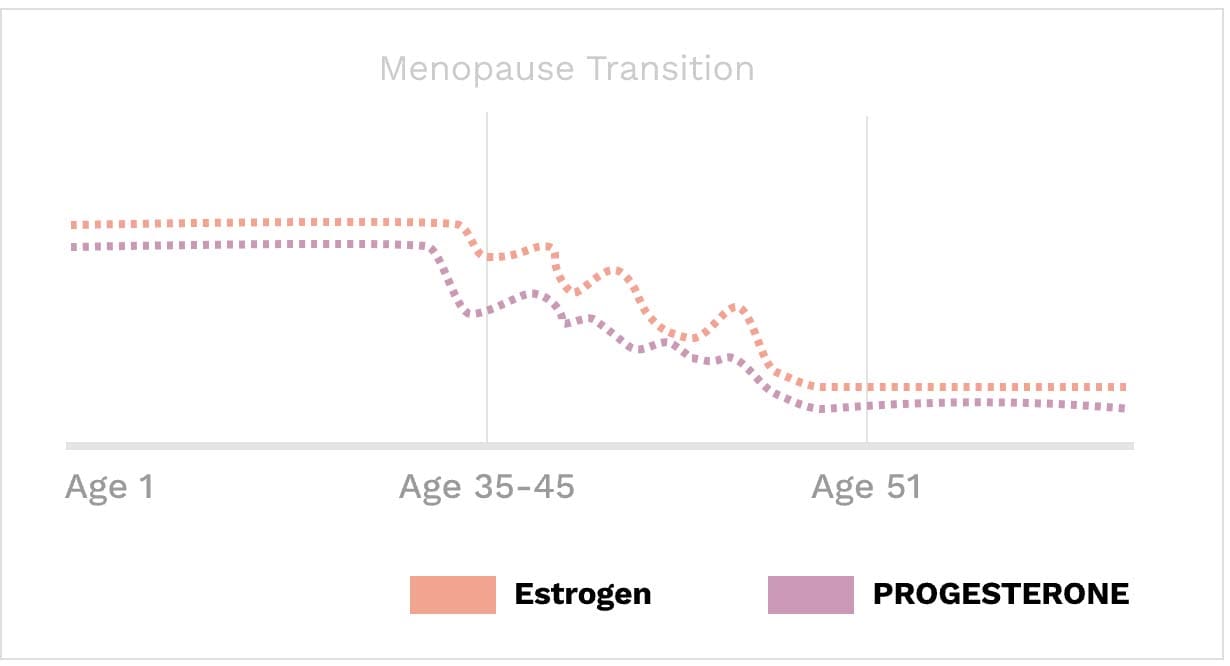 Estrogen & progesterone levels begin to drop around age 35, as women enter Perimenopause. Healthy women enter full menopause around age 51. This time period comes with significant changes in mental, emotional, and physical health. Women with good foundational health experience this transition gradually and with only minor symptoms.
Estrogen & progesterone levels begin to drop around age 35, as women enter Perimenopause. Healthy women enter full menopause around age 51. This time period comes with significant changes in mental, emotional, and physical health. Women with good foundational health experience this transition gradually and with only minor symptoms.Measuring Hormones
While measuring hormones in the blood can be helpful, we use several methods of testing hormones to get a full picture of your hormonal health. This is because some hormones can be seen better in the blood, while other hormonal metabolites are easier to measure in the saliva or the urine.
It is also essential to know when to test specific hormones. Women have fluctuations in their sex hormones and testing at the wrong time of day or the wrong day of the month can result in information that is difficult to interpret. We typically test women’s hormones twice during one cycle. The menstrual cycle is counted starting with day 1 as the first day of a woman’s period. We often test around day 5 of the menstrual cycle to look at levels of estrogen, LH, and FSH. Then we test again at day 19-21 to examine progesterone levels since this is when progesterone should be peaking if ovulation has occurred.
Menopausal Hormone Testing:
Testing hormones post-menopause can still be important but is much different. Because hormone levels flatten out, we use an individualized approach with each client for testing post-menopause based on your symptoms.
KEY HORMONES FOR WOMEN:
Important Levels Of Estrogen
There are three primary forms of estrogen we can measure, each of which is needed in different proportions at different stages of life.
Estrone (E1)
E1 is primarily made in the ovaries before menopause. Although total estrogens decline overall around menopause, estrone becomes the dominant circulating estrogen and is principally made in fat tissue post-menopause.
Estradiol (E2)
Estradiol is the most potent estrogen during reproductive years in terms of absolute levels and impacts. Estradiol influences female secondary development such as breasts and fat distribution. It also helps maintain reproductive tissues like the ovaries and lining of the uterus. E2 impacts endometriosis and fibroid development. It also supports bone growth, heart health, and memory.
Estriol (E3)
E3 is secreted as the dominant estrogen during pregnancy. Levels of estriol in women who are not pregnant are almost undetectable.
Important Levels Of Progesterone
Progesterone plays a crucial role in female fertility and reproductive function, and increases significantly during pregnancy. Progesterone levels in a pregnant woman can reach ten times that of a non-pregnant woman. However, Progesterone has many other functions that aren't widely recognized. Progesterone is secreted by the ovaries to prepare the inner lining of the uterus for pregnancy. It also inhibits muscular contractions that prevent the egg's adherence to the uterine wall. If an egg is not fertilized, the ovaries will cease secreting progesterone.
High Progesterone Levels May Indicate:
- Pregnancy
- A cyst in the ovaries
- A disorder in the adrenal glands (rare)
- Ovarian cancer (rare)
- Excessive levels of stress
Lower Progesterone Levels May Indicate:
- Ectopic pregnancy
- Miscarriage
- Irregular Cycle
- Absence of menstruation (amenorrhea)
Important Levels Of Testosterone
Testosterone is not just a hormone for men. Optimized levels are essential for energy production, maintaining muscle, preventing fat storage, reproductive function, and libido.
Low testosterone levels can cause chronic unexplained fatigue, a decreased sense of personal well-being, and low libido in women. Additional symptoms include muscle weakness, depressed mood, and weight gain. Additionally, low levels have been linked to the following:
- Bone loss
- Muscle wasting
- Obesity
- Depression
- Breast cancer
Important Levels Of Cortisol
Cortisol is known as "the stress hormone." It’s a crucial hormone, as chronically high cortisol levels are associated with nearly every major chronic disease. Measuring cortisol is complex, as it’s interrelated with many other hormones including melatonin levels and testosterone.
Cortisol levels fluctuate throughout the day, peaking in the morning and decreasing throughout the day. Salivary lab cortisol markers can range depending on when the sample was taken. For most tests, the average blood cortisol ranges are:
- 6 a.m. to 8 a.m.: 10 to 20 micrograms per deciliter (mcg/dL).
- Around 4 p.m.: 3 to 10 mcg/dL.
Key Factors In Balancing Hormones
Hormones are cyclical and highly delicate. One imbalance can trigger a cascade of other imbalances. Taking a reductionist approach that focuses too much on a single hormone can often lead you to more and more confusion. We help our clients develop a holistic approach that addresses all the underlying causes of imbalance, trusting in good foundational health habits. We help our clients simplify their regimens and focus on the essentials that have been proven to help balance hormones over the long-term.

TARGETS FOR CORRECTING THE IMBALANCE:
1. Metabolic dysfunction
Insulin resistance, prediabetes, diabetes and other disorders of metabolism can be the root cause for some hormonal imbalances such as polycystic ovarian syndrome (PCOS). Women are significantly more susceptible to insulin imbalances, and this is often one of the first places we look to address hormone imbalances. Research has demonstrated a significant impact between hormone imbalances and insulin insensitivity (7).
2. Inflammation
3. Stress
4. Environmental Toxins
5. Genetics
SOURCES
- Mohan MP, Ramesh TC. Multiple autoimmune syndrome. Indian J Dermatol Venerol Leprol. 2003;69:298–299.
- Kwak, Yeunhee, Yoonjung Kim, and Kyoung Ah Baek. “Prevalence of irregular menstruation according to socioeconomic status: A population-based nationwide cross-sectional study.” PloS one 14.3 (2019): e0214071.
- Remission of Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders. http://noetic.org/wp-content/uploads/2020/10/SRB-chapter12.pdf
- Biancone, Livia, et al. “Treatment with biologic therapies and the risk of cancer in patients with IBD.” Nature Clinical Practice Gastroenterology & Hepatology 4.2 (2007): 78-91.
- Brown, E. Sherwood, et al. “Effects of chronic prednisone therapy on mood and memory.” Journal of affective disorders 99.1-3 (2007): 279-283.
- Puckett, Yana, Aishah Gabbar, and Abdullah A. Bokhari. “Prednisone.” (2018).
- Zsuzsanna, Suba . “Interplay between insulin resistance and estrogen deficiency as co- activators in carcinogenesis” (2012)
- Eline S. van der Valk, et al. Stress and Obesity: Are There More Susceptible Individuals?.2018.

Schedule an info call to learn more or register for your Wisdom Care Program
Have questions? Schedule a free info call today with one of our care coordinators.
