Autoimmunity
How Autoimmunity Develops: Chronic Inflammation
You can think of this like a glass of water…
Glass Of Water Analogy

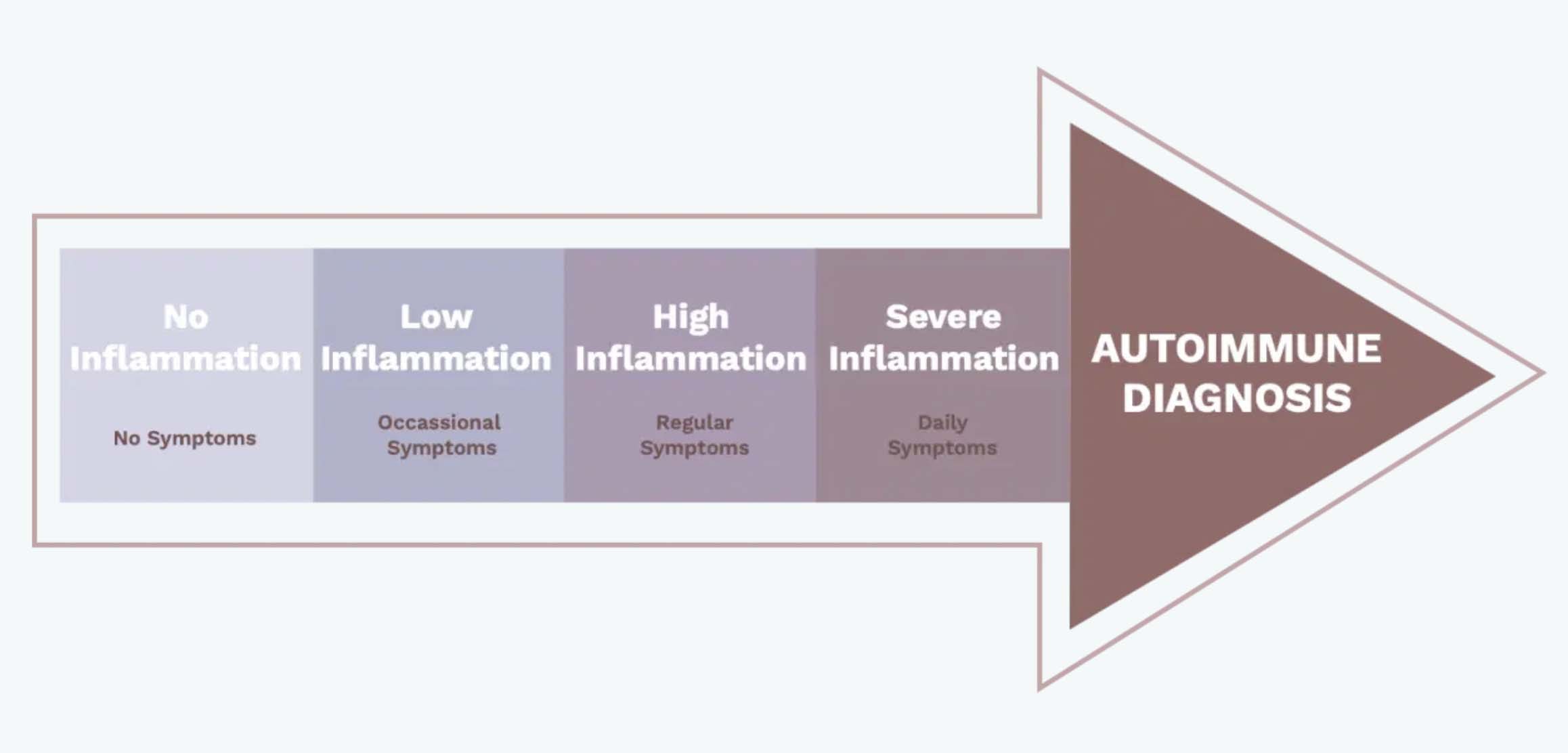
Autoimmunity Is A Spectrum
Lower-severity autoimmune conditions are correlated with lower overall inflammation, whereas more severe autoimmune conditions indicate higher levels of inflammation. You can move up and down that spectrum depending on your overall inflammation, which is why symptoms of autoimmune seem to mysteriously disappear and reappear. It’s also why if you receive an autoimmune diagnosis, you’re 3x more likely to receive a second (1).
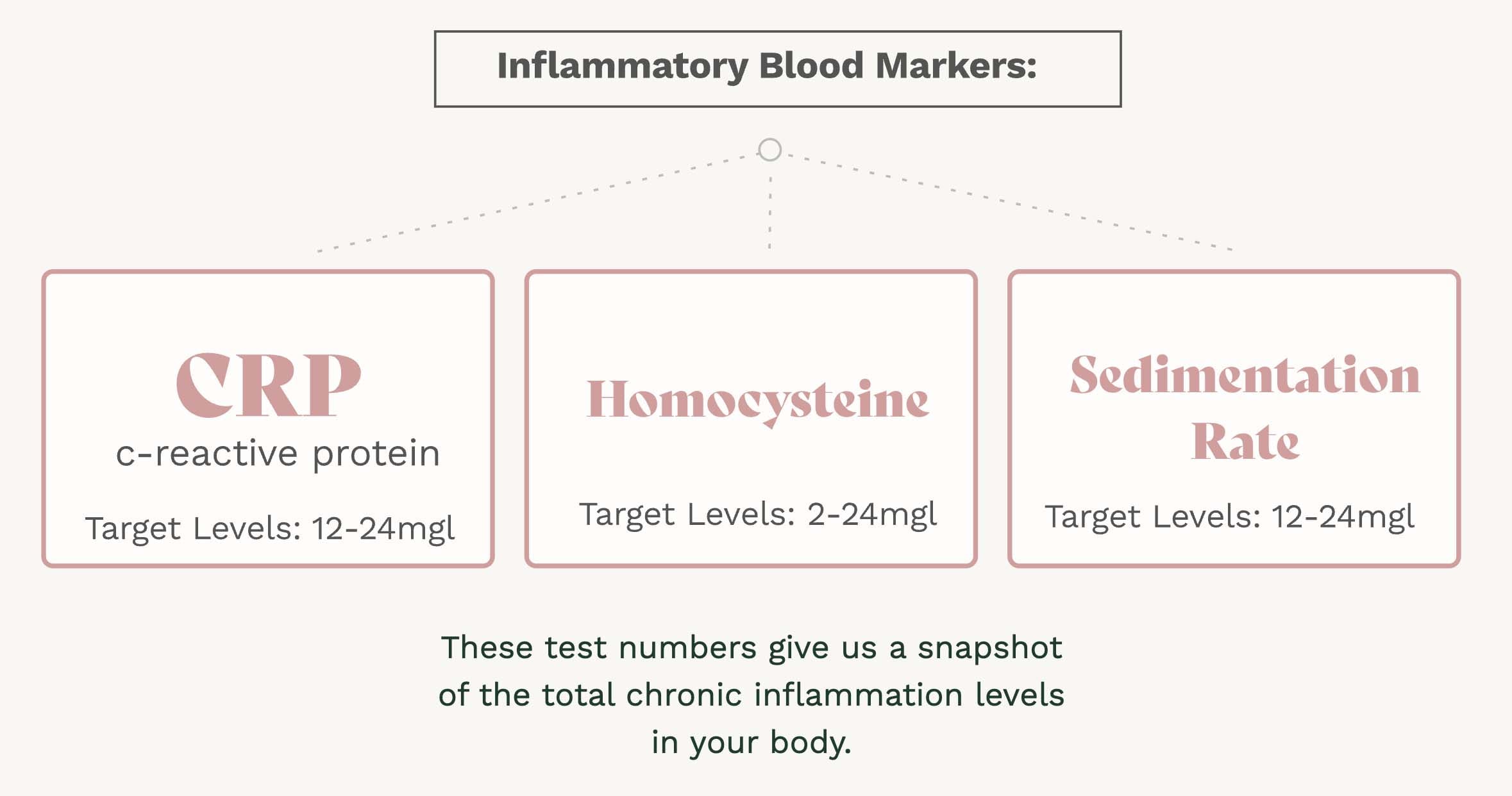
Measuring Autoimmunity
Breakthrough research demonstrates autoimmunity is highly correlated with inflammatory blood markers like C-Reactive Protien, homocysteine, and sedimentation rate. The more inflammatory markers in the blood, the greater the likelihood of autoimmune symptoms. Consistently high inflammatory markers are often referred to as chronic inflammation.
Inflammatory levels in the blood naturally fluctuate and are primarily influenced by lifestyle. This means you can significantly reduce inflammatory levels and autoimmunity, even to the point of complete remission.
Lower Inflammation, Lower Autoimmunity
No matter which of the 100+ autoimmune diagnoses received, addressing the underlying inflammation addresses the root cause of autoimmunity and reduces the likelihood of all symptoms.

SOURCES OF INFLAMMATION:
1. Hidden Food Sensitivities
Some food allergies create immediate, intense bodily reactions such as a severe peanut allergy. However, most people live with food sensitivities that go unnoticed. These are lower-grade immune reactions that often don’t occur for hours or days after you eat, making them difficult to detect. Fortunately, we can now run advanced tests for food sensitivity if you suspect you have one.
2. Gut Dysbiosis / Bacterial Imbalance
Everything you eat is processed by your microbiome; they eat what we eat. Different strains of gut bacteria produce different chemicals, which means the makeup of your biome is almost as important, if not equally important, as what you eat. When your gut biome is out of balance, it can transform food that is usually non-inflammatory, and create excessive inflammatory chemicals sent into your blood.
3. Infections
Previous viral infections like Epstein Barr, cytomegalovirus, and herpes simplex can become reactivated leading to chronic inflammation. These infections can be identified and dealt with by your Wisdom doctor.
4. Chronic Stress
While short-term stress exposure can be healthy (think exercise), lower levels of ongoing stress can exacerbate inflammation. Chronic stress has been proven to create inflammation and is linked to nearly every major chronic health issue, including autoimmunity.
5. Toxic exposure
Long term exposure to mold, pesticides, heavy metals and other environmental toxins can contribute to inflammation. These can be tricky to identify and treat, and should be done under the care of a doctor.
6. Metabolic Dysfunction
Eating highly processed foods combined with a lack of exercise can lead to obesity which can contribute to overall inflammatory levels.
When I was diagnosed with Multiple Sclerosis I was told that I would have to be on daily injections for the rest of my life, there was no hope. That was the scariest month of my life. Going to my doctors made me feel more scared as it was clear to me they didn’t have answers for me. Over the next year, I researched, changed my diet, and learned about all my inflammation triggers. Reversing them takes some time and effort, but I have completely reversed all my symptoms to the point of total remission.
SOURCES
- Mohan MP, Ramesh TC. Multiple autoimmune syndrome. Indian J Dermatol Venerol Leprol. 2003;69:298–299.
- Kwak, Yeunhee, Yoonjung Kim, and Kyoung Ah Baek. “Prevalence of irregular menstruation according to socioeconomic status: A population-based nationwide cross-sectional study.” PloS one 14.3 (2019): e0214071.
- Remission of Endocrine, Nutritional and Metabolic Diseases, and Immunity Disorders. http://noetic.org/wp-content/uploads/2020/10/SRB-chapter12.pdf
- Biancone, Livia, et al. “Treatment with biologic therapies and the risk of cancer in patients with IBD.” Nature Clinical Practice Gastroenterology & Hepatology 4.2 (2007): 78-91.
- Brown, E. Sherwood, et al. “Effects of chronic prednisone therapy on mood and memory.” Journal of affective disorders 99.1-3 (2007): 279-283.
- Puckett, Yana, Aishah Gabbar, and Abdullah A. Bokhari. “Prednisone.” (2018).
- Zsuzsanna, Suba . “Interplay between insulin resistance and estrogen deficiency as co- activators in carcinogenesis” (2012)
- Eline S. van der Valk, et al. Stress and Obesity: Are There More Susceptible Individuals?.2018.

